If you partner with an effective IME vendor, the claimant will be sent to a physician who is highly qualified and skilled at performing these exams.
When claimants arrive for an IME, these physicians explain the purpose of the exam and that it was requested by the insurance company (or payer). They inform claimants that they’ve spent significant time reviewing their medical files, that they’re going to perform an evaluation and provide the findings to the requesting company. If claimants want a copy of the results, they can obtain it from the insurer.
Although IME physicians are not facilitating treatment, a quality IME still provides significant benefits to injured workers. In many cases, the IME physicians may uncover medical issues previously overlooked, or they may connect the dots to figure out underlying issues or even solve a previously unexplained medical mystery. As a result, the IME can lead to injured workers getting the treatment they need sooner, which is a significant benefit to their well-being.
The Physician Perspective: Expert Opinions Based on Reasonable Medical Certainty
In this Part 3 of our series on quality IMEs, we interviewed two premier physicians to get their thoughts on what constitutes a quality IME process.
“For me, preparing for an IME starts three or four days before the actual exam,” said Amir Reza Moinfar, MD, of Elite Orthopaedic & Musculoskeletal Center. “I start by reviewing medical records. In some cases, these files can be on the order of up to several thousand pages. It’s a good opportunity to familiarize myself with the particular claim and to potentially catch items that may be missing from the file. For example, if I’m going to assess whether a claimant can return to full duty, I need the job description. If a claimant has had surgery, I need to most certainly have access to the operative note. There’s still time to request any missing information in advance of the exam. This helps to make the process, in my opinion, more seamless, thorough and efficient.
“When an IME physician gives an opinion, it needs to be based on medical evidence and based within a reasonable degree of medical certainty. There are legal ramifications that help hold an IME to a high standard,” explained Moinfar.
“There’s a certain skill set that’s required in performing these exams,” he added. “Much of it comes with experience, but a lot of it comes from proactively going out of your way to learn and become as proficient as possible in performing these exams. I chose not to perform IMEs straight out of training. First, I wanted to feel confident in my ability to treat patients and formulate decisions with their care. There are also legal terms an IME physician must become familiar with, such as causation, disability, impairment, and apportionment. These things aren’t taught in medical school, but a physician can take courses and study on the practice of performing quality IMEs. Also, I feel that a lot of the skills associated with performing IMEs come with experience.”
We also spoke with Ghazala Kazi, MD, MPH, of Medical Advisory Services. “I’m an occupational medicine physician so performing IMEs is my specialty,” she explained. “I’m trained to determine work-relatedness. I don’t always conclude that a condition is not related to work. In fact, most of time I conclude that it is work-related. With those cases, the insurer can proceed in providing the claimant with treatment. I’m helping the insurance company make a decision, and I’m helping the claimant, who may have been struggling for months, or even years, to get the care they need.”
She also discussed the importance of having a complete claimant medical record in order to determine causation: “The file should include the accident report and all relevant diagnostic tests, such as any MRI or CT scan reports. If I’m evaluating a claimant’s respiratory system, it’s critical to have the pulmonary function test reports. If there are tests conducted prior to the injury, it’s important to receive those reports as well. Let’s say I’m asked to determine if a person’s hearing loss is work-related. In that case, if a baseline test was performed at the time of employment, I need the results of that test to make the determination.
“Sometimes, if someone is injured, the mechanism of injury is obvious,” noted Kazi. “However, there are complex cases, where I have to review studies to determine if there is a causal relationship between the condition and the work environment. An IME physician who has the knowledge and training in epidemiology understands the methods to draw this conclusion and is trained to read such studies. Only a physician with the right expertise can perform this type of analysis.”
The method that Dr. Kazi is referring to is the Hills Criteria for Causation, a set of nine criteria that provide epidemiological evidence of the relationship between a presumed cause (e.g., a work-related accident) and the observed effect (the worker’s injury).
Bridging the Quality Divide
Over the course of our three-part series on IME best practices, we’ve outlined how you and your organization can bridge the divide and consistently obtain a quality IME result.
When looking for a place to initiate these changes, it’s essential to start at the beginning and refine the process by which you request these exams. From there, ensuring that you are utilizing a sophisticated IME vendor is another important step. A quality vendor is essentially the conduit to getting your injured workers matched to the best, most-qualified IME physicians – resulting in an IME that drives informed decisions and moves claims toward closure.
 MCN’s clinic calendars for April 2021 are available for our 20-plus clinic locations, which provide independent medical examinations and peer reviews throughout Washington and Oregon.
MCN’s clinic calendars for April 2021 are available for our 20-plus clinic locations, which provide independent medical examinations and peer reviews throughout Washington and Oregon.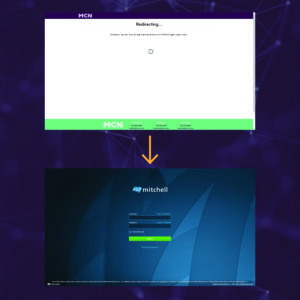 MCN’s client portal login page will be experiencing changes.
MCN’s client portal login page will be experiencing changes.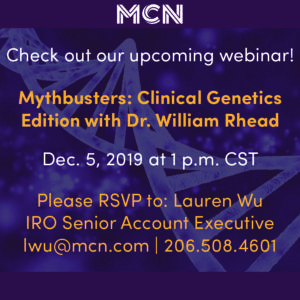 MCN’s IRO team will be hosting a complimentary webinar about genetics titled “Mythbusters: Clinical Genetics Edition with Dr. William Rhead.” This webinar takes place on Thursday, Dec. 5, 2019 at 1 p.m. CST. To RSVP, please reach out to Lauren Wu, IRO Senior Account Executive, at lwu@mcn.com or 206.508.4601.
MCN’s IRO team will be hosting a complimentary webinar about genetics titled “Mythbusters: Clinical Genetics Edition with Dr. William Rhead.” This webinar takes place on Thursday, Dec. 5, 2019 at 1 p.m. CST. To RSVP, please reach out to Lauren Wu, IRO Senior Account Executive, at lwu@mcn.com or 206.508.4601.



